The Future of Telemedicine: Regulatory Support and Technological Advances to Drive 25–30% of U.S. Medical Visits by 2026
By the end of 2026, 25–30% of all medical visits in the United States will be conducted via telemedicine. Although the adoption rate of telemedicine has been low in 2024, it will grow considerably with regulatory support from the US Congress.
ScienceSoft’s research team analyzed industry statistics, current developments and limitations in telehealth regulations, and opinions of healthcare community leaders to present a fresh perspective on the future of telehealth in the US.

Why You Shouldn’t Give Up on Telemedicine
Due to lockdowns enforced during the COVID-19 pandemic, the US health systems quickly adapted to remote health services, which allowed patients to receive care while minimizing infection risk. Federal regulations were relaxed, and telehealth reimbursement policies were expanded, encouraging providers to incorporate telemedicine services broadly.
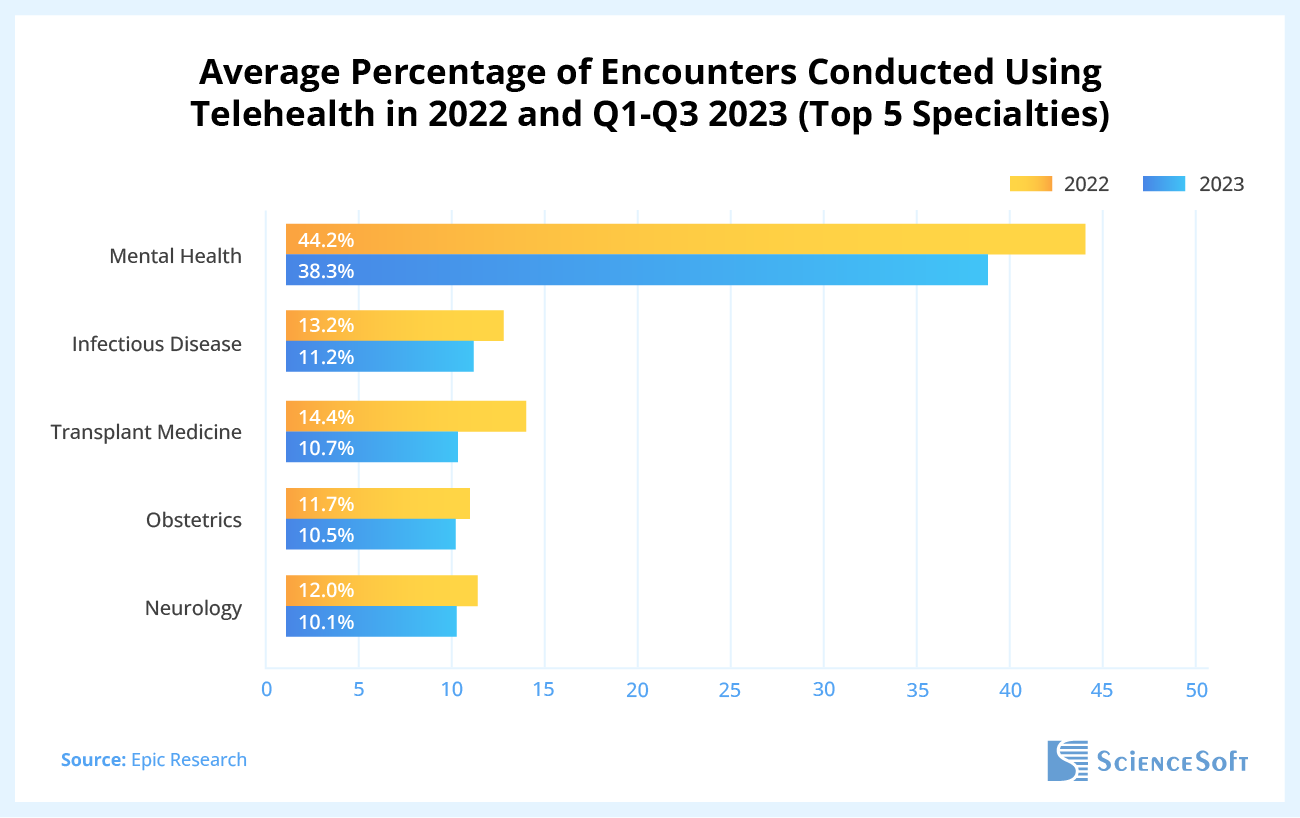
Fast-forward a couple of years, and the adoption of telehealth dropped to around 4 to 6% (as reported by CMS and Epic, respectively), even though its usage in the US remained at a higher level than before the pandemic. At the same, in some areas like mental health, the usage of telemedicine remained high: 38% of all mental health visits in 2023 were conducted remotely.
We believe that the resilient utilization in mental health shows that the necessary technology and demand are already in place. Key obstacles to telemedicine adoption are related to regulations rather than technological barriers or lack of demand. With the persistent efforts from the US medical community, the US Congress is likely to permanently extend and enhance the existing telehealth policies.
Key Setbacks and Drivers of Telehealth in 2025: Facts and Insider Opinions
Most US hospitals already have technology in place, but rural areas are struggling with slow internet connection
The slow adoption of telemedicine is definitely not a matter of telehealth availability. According to hospital technology implementation data from Definitive Healthcare, as of February 2024, 78.6% of hospitals in the United States had installed a telemedicine solution.
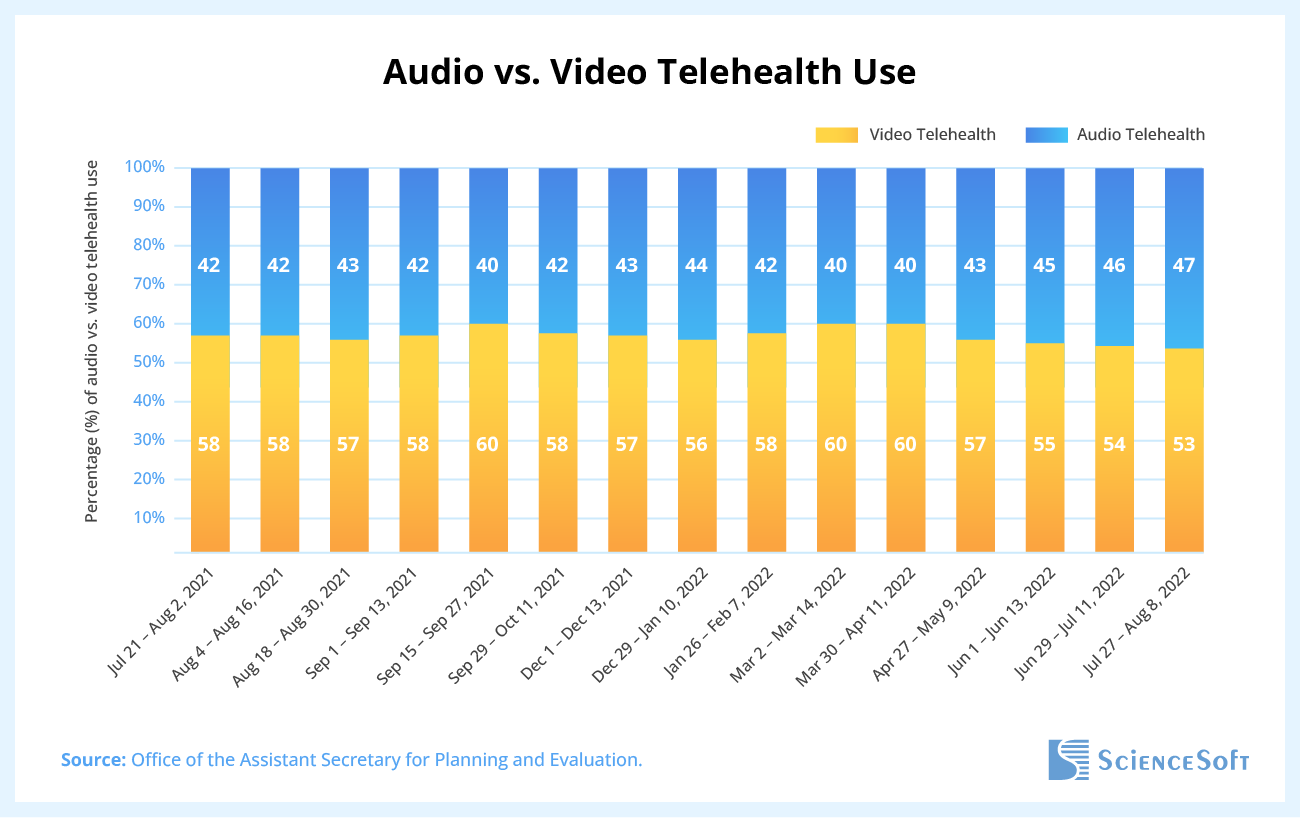
While hospitals have the necessary software in place, access to broadband remains a barrier for patients in rural and underserved areas. For these individuals, audio-only visits are just as important as video calls. In fact, data from the US Government Office of Health Policy reveals that nearly half of all telehealth appointments during July and August of 2022 were audio-only appointments.
The mental health sector leaps ahead in telemedicine adoption
In 2023, telemedicine usage in mental health was over three times higher than in other medical specialties, according to Epic Research. We believe that the resilient demand for telemedicine in mental health indicates that the technology is here to stay.
The persistent demand for online mental health services has fueled the attention of investors. According to the KPMG report on M&A activities in mental health services, private equity firms show interest in investing in telehealth platforms that offer mental health services.
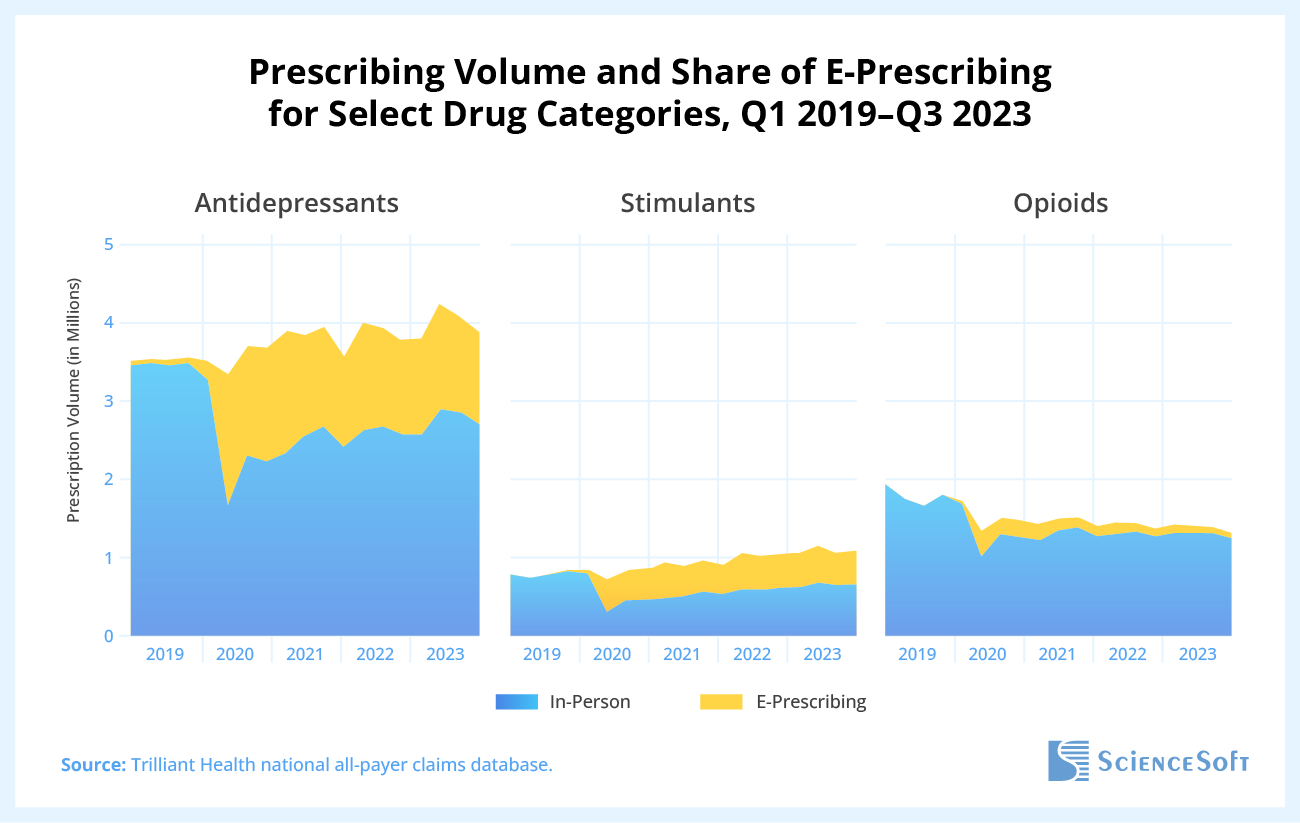
The growth in telemedicine usage during the pandemic stimulated the adoption of e-prescribing in mental health, and the trend has persisted even after the outbreak. According to Trilliant Health, in the third quarter of 2023, e-prescribing accounted for roughly one-third of anti-depressant prescriptions. With e-prescribing, patients with mental health issues can avoid unnecessary in-person visits that can trigger additional anxiety. This option is also essential for patients who can’t travel for frequent in-person visits due to barriers like distance, cost, childcare, or work obligations.
The main hurdle to telehealth growth in the US is lack of government support
After analyzing the regulatory landscape surrounding telemedicine, we came to the conclusion that the future of its adoption — whether it continues to increase or returns to pre-pandemic levels — largely depends on government decision-makers.
The relaxation of telehealth regulations introduced during the pandemic was extended through December 31, 2024. However, its fate is unclear as, according to the Congressional Budget Office, new extensions would result in $2B in excess Medicare spending. Nevertheless, we can see a collective effort from the healthcare community to permanently extend several telehealth policies beyond December 2024.
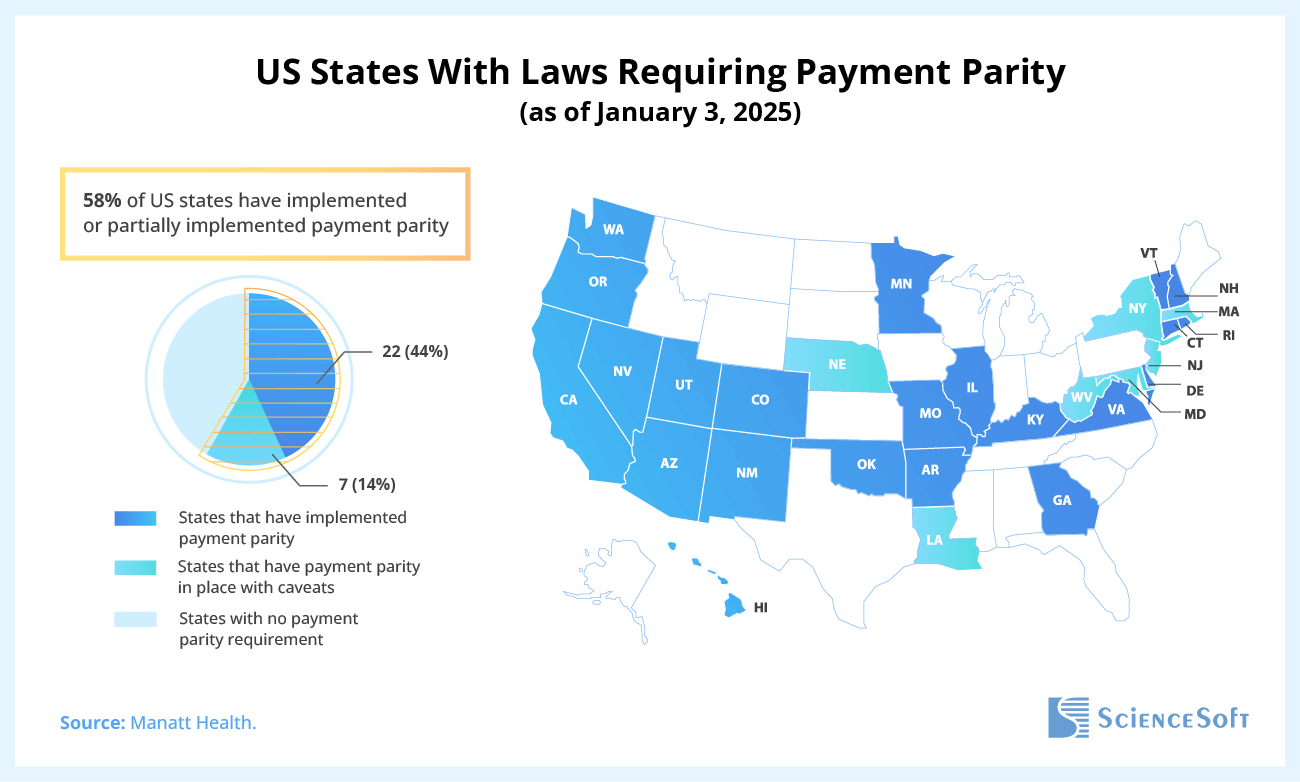
According to the AMA’s guide to the appropriate use of telemedicine, telehealth adoption is slowed by a lack of financial viability. In this regard, the state regulations are halfway to meeting the needs of the healthcare community. As of January 3, 2025, nearly half the US states had implemented payment parity policies, ensuring that telehealth services are reimbursed at the same rate as in-person visits. If the other states follow the general trend, that may become a push towards telemedicine adoption.
However, cross-state regulations remain a challenge for both patients and providers. According to the Cicero Institute, a nonpartisan public policy organization, as of January 2024, 27 US states (54%) didn’t allow practicing cross-state telehealth. The story of Maki Inada, a biology professor from New York, illustrates the impracticality of the situation: her Boston-based cancer specialists required her to be in Massachusetts for a telemedicine visit. The hospital suggested she could “just” drive five and a half hours to the state border and conduct the session from her car.
Industry representatives are cautiously optimistic about telehealth
Many experts in the industry believe that telemedicine adoption during the pandemic was unnatural, and in the future, it will be more gradual as society needs time to adapt to these changes. “It’s going to take another five years or so to see that go up to the 50% to 70% rate that we’ve seen during the early part of the pandemic”, predicts Eyal Zimlichman, chief innovation and transformation officer at Sheba Medical Center.
At the same time, there’s a growing interest in new ways of delivering care through telehealth innovations. Ateev Mehrotra, professor of health care policy at the Blavatnik Institute at HMS, believes that technological advances are slowly changing how we define the practice of medicine. A striking example of this transformation comes from Dubai, where healthcare provider Medcare recently launched its first hospital in the metaverse. As a digital twin of the physical hospital, it allows patients to experience its services before traveling to the physical space, including consulting with their doctors in VR.
How Telemedicine Transforms Healthcare in the Post-COVID Era: A Realistic Look
Providers see higher patient capacity and lower costs per visit
Telemedicine significantly optimizes resource use within healthcare facilities. Remote patient monitoring (RPM) enables providers to create an equivalent of at-home “virtual beds,” allowing them to treat more patients without increasing physical capacity. This model generates more revenue with the same or reduced resource usage. According to a report by McKinsey from May 2023, virtual hospitals in Australia reduced care costs by up to 19% thanks to telemedicine.
Furthermore, telemedicine smooths the patient flow by offering greater flexibility in scheduling. Rather than contributing to peak demand in the mornings and evenings, patients can book appointments throughout the day, creating a more balanced workload for providers.
At the same time, with the rise of telemedicine, senior healthcare professionals who have practiced for decades in a traditional, face-to-face model of care may face the challenge of adapting to new technologies. To support this transition, healthcare organizations will need to implement efficient, accessible training programs that help these practitioners build confidence in using telehealth tools. Ensuring that telemedicine platforms have user-friendly and intuitive design is another way to minimize technological barriers and cognitive load for clinicians.
Author's note: I see that many physicians whom I interview as part of my work remain cautious about fully embracing telemedicine. All regulatory hurdles aside, they are sometimes unwilling to recommend remote consultations to their patients due to the risk of missing critical symptoms that might be more apparent in an in-person exam. From my perspective, it’s important to strike a balance here. For routine follow-ups, medication refills, mental health consultations, or minor ailments like colds and flu, virtual visits can be an excellent way to save time and reduce strain on the healthcare system. However, for more complex or urgent issues (e.g., acute pain), an in-person visit is crucial for an accurate diagnosis and immediate intervention.
Patients enjoy higher care accessibility but face the risk of alienation without in-person visits
Telemedicine makes care more accessible for rural and underserved areas where physical facilities are scarce. If cross-state regulations become more flexible, patients’ choices will expand with specialty care and providers outside their geographic location.
Reduced travel to healthcare facilities means less exposure to potential health risks for patients and those they might encounter during their journeys. Patients with chronic conditions can benefit from continuous monitoring and regular check-ins, helping them manage their health proactively. Additionally, online consultations can provide a degree of anonymity not available during in-person visits, a key advantage for patients seeking help in socially stigmatized areas such as mental health.
However, telemedicine does come with challenges. The biggest one is the potential reduction in the overall quality of care. Overreliance on technology may lead to patient reluctance to visit the hospital in person, which could prevent caregivers from noticing critical signs of disease that are best detected through physical examinations. This lack of face-to-face interaction may also lead to patients not feeling as accountable for following the prescribed treatment plans as they might with traditional family medicine.
Payers reduce claim severity at the cost of lower transparency
Increased care accessibility makes preventive check-ups and health monitoring more convenient and affordable for patients, which may encourage them to seek regular care. As a result, insurers could see a reduction in the frequency and severity of claims, particularly if telemedicine helps to reduce costly emergency room visits for non-urgent issues. In this way, telemedicine holds the potential for substantial cost savings in claim payouts.
However, telemedicine also presents some risks for insurers. The remote nature of telehealth allows opportunities for false claims, as it is more difficult to verify whether a telemedicine visit truly occurred.
ScienceSoft is a US-based healthcare IT consulting and software engineering company with 20 years of experience in the domain. We deliver compliant patient-centric solutions tailored to different medical specialties such as neurology, pediatrics, primary care, and more.

